Disclaimer: Not everyone who goes through menopause identifies as a woman and not all people who identify as women go through menopause. At Jayla, our core audience is people who identify as women, so we primarily use the word “women.” However, we’re working on specific content for people going through menopause who might not identify as women. Inclusivity is a key value of ours, so bear with us!
What’s the Deal With Hormone Replacement Therapy
Your friend swears by hormone replacement therapy? But your sister warned you of potential negative side effects? And your doctor barely spoke about it?
Are you unsure of what hormone replacement therapy even is?
The dialogue around hormone replacement therapy (HRT) is confusing and convoluted. That leads many women to simply “deal with” their menopause symptoms, rather than explore how HRT could potentially help them. But this doesn’t have to be the case. Here are the key facts you should know about HRT.
What is Hormone Replacement Therapy (HRT)?
Hormone replacement therapy (HRT) is a treatment used to help manage menopause symptoms. It supplements the hormones estrogen and/or progesterone, which decrease as you approach menopause.
What are hormones?
Hormones are messengers made by your endocrine glands. They travel around your body and tell different parts what to do and when to do it.
During perimenopause and menopause, our bodies’ levels of estrogen and progesterone (the primary female reproductive hormones) naturally decline. This impacts our entire body – from mood and sleep to metabolism and sex drive. HRT maintains our hormone balance by replenishing these hormones. By supplementing hormone levels, HRT reduces the symptoms that hormonal fluctuations can cause (hot flashes, irritability, anxiety, all those fun things you’ve heard of!).
HRT is also known as menopausal hormone therapy or estrogen replacement therapy.
Progesterone
Is a natural hormone produced by the body, crucial for regulating the menstrual cycle and supporting pregnancy.
Progestogens
Include both natural (like micronized progesterone) and synthetic compounds, used in contraception and hormone replacement therapy.
Progestins
Are a subset of synthetic progestogens specifically designed to mimic progesterone’s effects, used in birth control and less commonly hormone therapies.
What are the types of HRT?
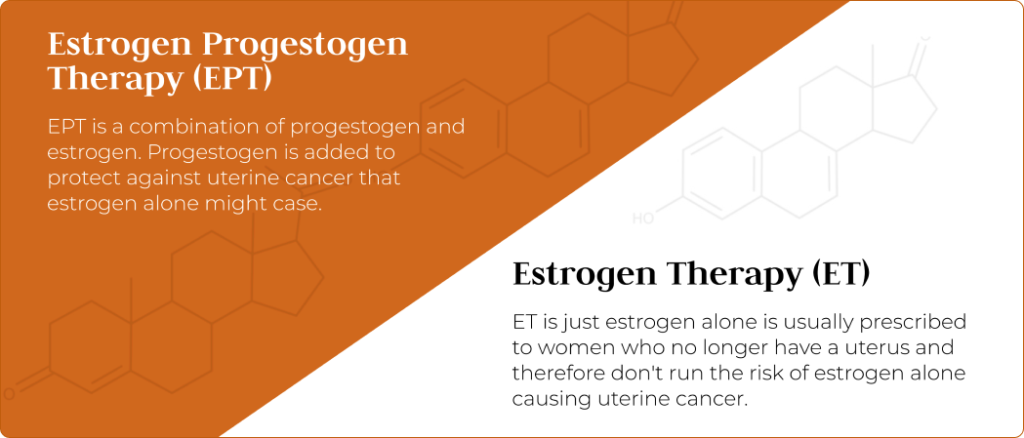
There are two primary types of HRT. The most commonly used HRT is estrogen plus progestogen therapy (EPT), followed by estrogen-only therapy (ET).
Estrogen plus progestogen therapy (EPT)
EPT releases progestogen and estrogen into the bloodstream or vaginal tissue, to replenish these hormones. Estrogen is the hormone that provides the most relief from menopausal symptoms. Progestogen is added to safeguard women against uterine (endometrial) cancer that estrogen alone might cause.
If you have not had a hysterectomy (removal of the uterus), your physician will typically recommend this form of therapy.
Estrogen-only therapy (ET)
ET is usually prescribed to women who have had a hysterectomy and no longer have a uterus. Women who no longer have a uterus don’t run the risk of estrogen alone causing the lining of the uterus to grow, thereby increasing the risk of endometrial cancer.
If you don’t have a uterus, you run zero risk of uterine cancer so there’s no need to add progestogen. That’s why only estrogen is prescribed.
What symptoms does HRT treat?
We have estrogen receptors all over our bodies, which is why menopause symptoms are numerous and varied.
Given that HRT supplements your hormone levels during a time when they are decreasing, HRT treats a significant number of menopause symptoms:
- Hot flashes
- Night sweats
- Mood changes, such as irritability
- Vaginal dryness or discomfort during intercourse
- Urinary incontinence or frequent urination
- Insomnia or sleep disturbances
- Joint pain
- Memory problems
Sounds too good to be true? Many women have said HRT transformed their lives. However, trust in HRT has waxed and waned. Additionally, HRT’s effects are dependent on the type, form, timing of first use, and other factors (1), so it’s not one size fits all.
HRT may also help with depression, anxiety, and weight gain, but other potential treatments may be more fitting. It’s important to speak with a clinician. Before we get into the benefits of HRT, we’ll first consider some of the concerns.
Why has HRT come under scrutiny?
HRT received criticism over the years, and that’s led to only one in 10 women who could benefit from HRT actually taking it (2).
HRT faced its greatest wave of critique following a 2002 Women’s Health Initiative (WHI) study which suggested that HRT (specifically EPT type HRT) increased the risk of breast cancer and heart disease (3). This led to a drastic reduction in HRT prescriptions by doctors (and justifiably so) and in women taking HRT.
Is HRT bad for you?
Hormonal treatments can sometimes be perceived as “unnatural” and therefore bad for you, whether that be the contraceptive pill or HRT. Given the potential side effects of some hormones, that’s understandable.
Since 2002, much more research has been done around HRT (4). The short answer to whether or not HRT could be bad for you is: it depends, it could be great for you too. If accurately dosed and prescribed, the potential benefits often outweigh the risks (5).
Recent studies have shown that HRT could actually reduce the risk of heart disease, but still may affect the risk of breast cancer. However, the leading authority on menopause research, the North American Menopause Society (NAMS) found that the increased risk is very low (5). To put this in perspective, drinking five glasses of wine every week increases your risk of breast cancer by a lot more.
Moreover, the kinds of synthetic progestin hormones that were studied are no longer commonly prescribed. The majority of progesterone prescriptions today are micronized progesterone, which has been observed to have reduced risks (5).
Other risks of HRT include stroke and blood clots. Your risk depends on your age, medical history, the hormones you use, and how you take them. A clinician who specializes in menopause care can help you optimize treatment and minimize certain risks. For instance, using estrogen patches on your skin reduces the risk of stroke and blood clots compared to taking estrogen by mouth (6).
Does HRT delay menopause?
In short: no. HRT does not delay menopause. Rather, it can help you manage menopause symptoms by supplementing the hormones that naturally decrease during menopause.
What are the benefits of HRT ?
First and foremost, you don’t feel like you’re losing your head with menopausal symptoms (hooray!). That’s a benefit that’s hard to measure, but given that symptoms can last more than 10 years, it can be pretty impactful.
Beyond menopause symptom relief, there are also other potential health benefits:
- Reduced risk of osteoporosis: a key risk in menopause is reduced bone density. This can sometimes lead to osteoporosis, a medical condition in which bones weaken and become more prone to the risk of fracture (6).
- Reduced risk of weight gain: as you likely know, weight gain increases the risk of heart attack, high blood pressure, stroke, and diabetes. Although more research is needed, HRT lowers the risk of weight gain, which in turn likely reduces the risks associated with weight gain.
How do I know if HRT is right for me?
Unless you’re someone who should not take HRT (see below), your best bet is working with a menopause clinician who knows how to prescribe and work with you to get the optimal, lowest dose that would be effective. You may have to adjust the dosage or form of HRT for optimal effect, but a menopause clinician can help you navigate the process. If the side effects of HRT are too great for you, you may feel that it’s not worth it.
If your menopause symptoms are impacting your life, we recommend talking to a menopause clinician who will help you determine whether HRT is right for you. Don’t forget to keep checking in with a clinician when taking HRT: they will work with you to determine if HRT is suitable for you, establish the appropriate dosage, and provide ongoing support to manage your treatment through each stage of menopause.
What are the side effects of HRT?
The common side effects of HRT might remind you of PMS symptoms: breast tenderness, feeling bloated, mood swings, headaches, and vaginal bleeding or spotting irregularly (7).
If any of these symptoms are severe, or if you experience other concerning side effects, it is important to discuss them with your clinician. Adjusting your dosage or switching to a different form of HRT, like changing from pills to patches, could help alleviate these issues quickly.
What form of HRT should I take?
The good news is that there are many different forms of HRT, and you can take them based on your specific needs.
HRT pills
Estradiol pills are taken once a day, with dosages of 0.5 mg, 1 mg, or 2 mg, based on your clinician’s advice. If you have a uterus, you’ll also need to take progesterone to protect your uterine lining.
A good option if you:
- don’t smoke
- don’t have issues with blood pressure, clotting, heart, or liver disease
HRT patches
Estradiol patches are convenient because you only need to remember to change them twice a week!
A good option if you:
- smoke
- are overweight
- have hypertension or migraines
- have a family history of stroke or heart disease
HRT gels
Absorbed through the skin, gels help with hot flashes, night sweats, mood changes, and vaginal symptoms.
Your clinician will guide you on the best option for your specific symptoms.
A good option if you:
- have bad reactions to patches
- don’t like the visibility of patches
- need to increase or decrease the dose easily
- want to increase your bone density
HRT vaginal creams (and suppositories)
Estradiol vaginal creams are for symptoms such as:
- Vaginal dryness
- Vaginal itching
- Vaginal burning
- Painful sex
- Frequent Urinary Tract Infections (UTIs)
- Urinary Urgency
A good option if you:
- want to target vaginal symptoms
- want to minimize common HRT risks as the medicine is hyper-targeted
They’re applied directly to the vaginal area and are used for bladder control issues, vaginal dryness, and pain during sex, rather than systemic symptoms like hot flashes or night sweats. Initially, you use the cream every other day, then less frequently after the first few months. Topical estrogen is typically prescribed daily for two weeks and then used twice weekly thereafter.
Who should not take HRT?
Hormone replacement therapy can be helpful for many women, but it might not be the best choice if you’ve had certain health problems in the past.
HRT is usually not recommended if you’ve previously experienced (8):
- A stroke or blood clotting event such as pulmonary embolism or deep vein thrombosis (DVT)
- Breast, ovarian, or uterine cancer
- Heart disease
- Untreated high blood pressure
- Liver disease
As mentioned above, some studies suggest HRT might raise the risk of breast cancer particularly. So if you’ve had breast cancer before, doctors generally recommend avoiding HRT. However, your doctor may still recommend topical estrogen for vaginal dryness and painful sex due to its lower risk profile.
What are the alternative options to HRT?
If you can’t or don’t want to take HRT, there are other options available. The FDA has approved three non-hormonal treatments:
- Fezolinetant (Veozah) for moderate to severe hot flashes (9)
- Paroxetine (Brisdelle) also for moderate to severe hot flashes (10)
- Ospemifene (Osphena) for painful sex due to menopause-related changes
Lifestyle approaches and over-the-counter products may help with distinct symptoms:
- Hot flashes: you might find relief by cutting back on caffeinated drinks and alcohol and trying relaxation techniques such as paced breathing.
- Vaginal issues, like dryness or painful sex: consider using a vaginal moisturizer or lubricant to ease discomfort
- You can also adjust your lifestyle and dietary habits to reduce the risk of symptoms and health issues. For instance, eating foods high in calcium and vitamin D or taking supplements with these nutrients can help prevent osteoporosis.
- Weight-bearing exercises such as weighted lunges and squats can also help maintain bone density and reduce the risk of osteoporosis.
How do I start HRT?
At Jayla, we’re committed to responsible HRT treatment. That means equipping women with accurate information, personalizing treatment courses, and scheduling appropriate follow-up visits.
To find out whether HRT is for you, follow these simple steps:
- Order the Jayla Menopause Kit to gain clarity into your hormone levels
- Book a free consultation with a Jayla menopause clinician to go over your hormone testing results, symptoms, and medical history
- Create a personalized treatment plan with your menopause clinician, which may include HRT if it’s suitable for you.
- If HRT is deemed suitable, your menopause clinician will prescribe HRT, and it will be delivered right to your door.
References
- Is HRT safe to use for the menopause? what the Science says (no date) University of Oxford. Available at: Source. (Accessed: 21 June 2024).
- Cumming GP; Currie H; Morris E; Moncur R; Lee AJ; (no date) The need to do better – are we still letting our patients down and at what cost?, Post reproductive health. Available at: Source (Accessed: 21 June 2024).
- Writing Group for the Women’s Health Initiative Investigators (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women, JAMA. Available at: Source (Accessed: 21 June 2024).
- Cagnacci, A. and Venier, M. (2019) The controversial history of Hormone Replacement therapy, Medicina (Kaunas, Lithuania). Available at: Source (Accessed: 21 June 2024).
- Breastcancer.org (2022) North American Menopause Society updates position statement on hormone therapy, says benefits outweigh risks for some women, Breastcancer.org – Breast Cancer Information and Support. Available at: Source (Accessed: 02 July 2024).
- Hormone therapy benefits may outweigh risks for many younger menopausal women (2023) News. Available at: Source (Accessed: 21 June 2024).
- (2022) Bioidentical hormones: Therapy, uses, Safety & Side effects, Cleveland Clinic. Available at: Source (Accessed: 21 June 2024).
- Files, J.A., Ko, M.G. and Pruthi, S. (2011) Bioidentical hormone therapy, Mayo Clinic proceedings. Available at: Source (Accessed: 21 June 2024).
- Shaukat, A. et al. (2023) ‘Veozah (Fezolinetant): A promising non-hormonal treatment for vasomotor symptoms in menopause’, Health science reports. Available at: Source. (Accessed: 02 July 2024).
- Carroll, D.G., Lisenby, K.M. and Carter, T.L. (2015) Critical appraisal of paroxetine for the treatment of vasomotor symptoms, International journal of women’s health. Available at: Source (Accessed: 02 July 2024).
- Ospemifene (Osphena) (2022) National Center for Biotechnology Information. Available at: Source. (Accessed: 02 July 2024).